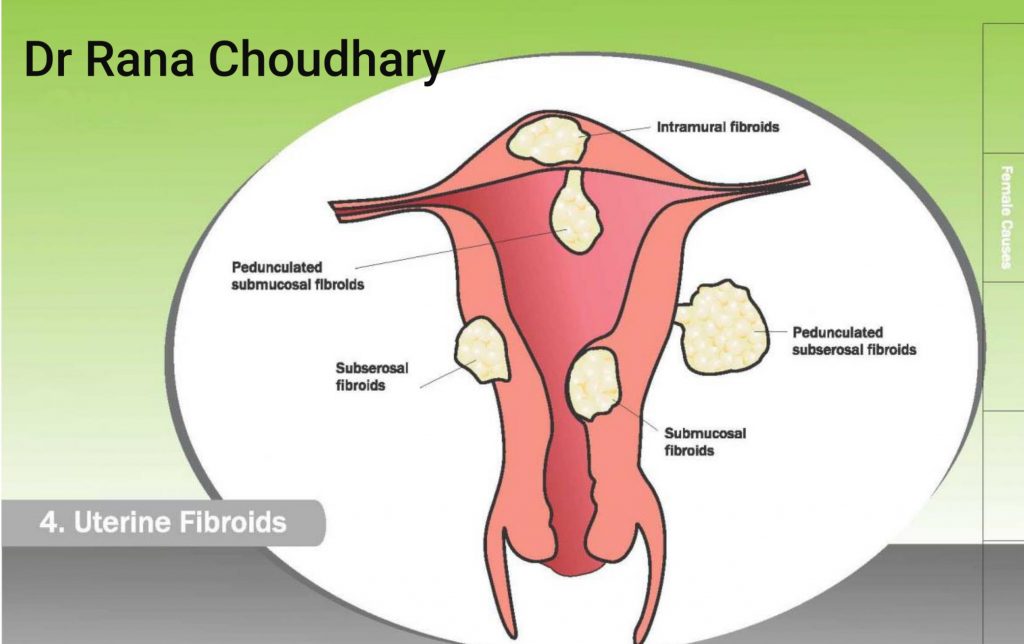
FIBROIDS
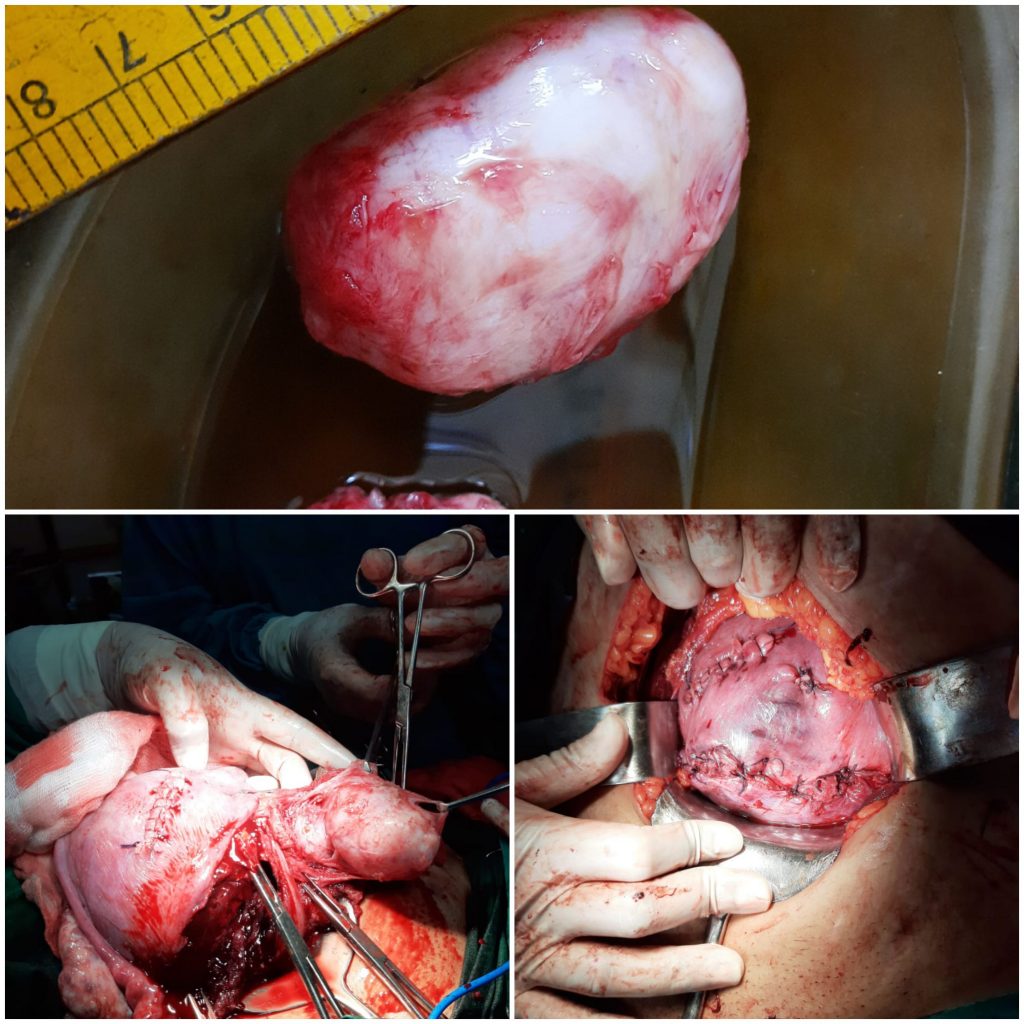
- Fibroids are mostly benign growth (tumor) in the uterus (womb). Very rarely a fibroid can turn malignant.
- If the size of submucous fibroid is small, medical therapy can be tried only in symptomatic women.
- For fibroids larger than 4 cm, its better to remove them surgically. Sometimes smaller but symptomatic fibroids also warrant removal eg those causing heavy bleeding etc.
- A fibroid can be diagnosed by ultrasonography, HSG, MRI etc. USG is the most common mode of diagnosis.
- Plan of surgery (LAPAROSCOPY OR HYSTEROSCOPY) is decided pre operatively depending upon the following factors:
- Location of fibroid
- Distance from serosa ( outermost layer of uterus) & mucosa ( innermost layer of uterus )
- Number and site of incision
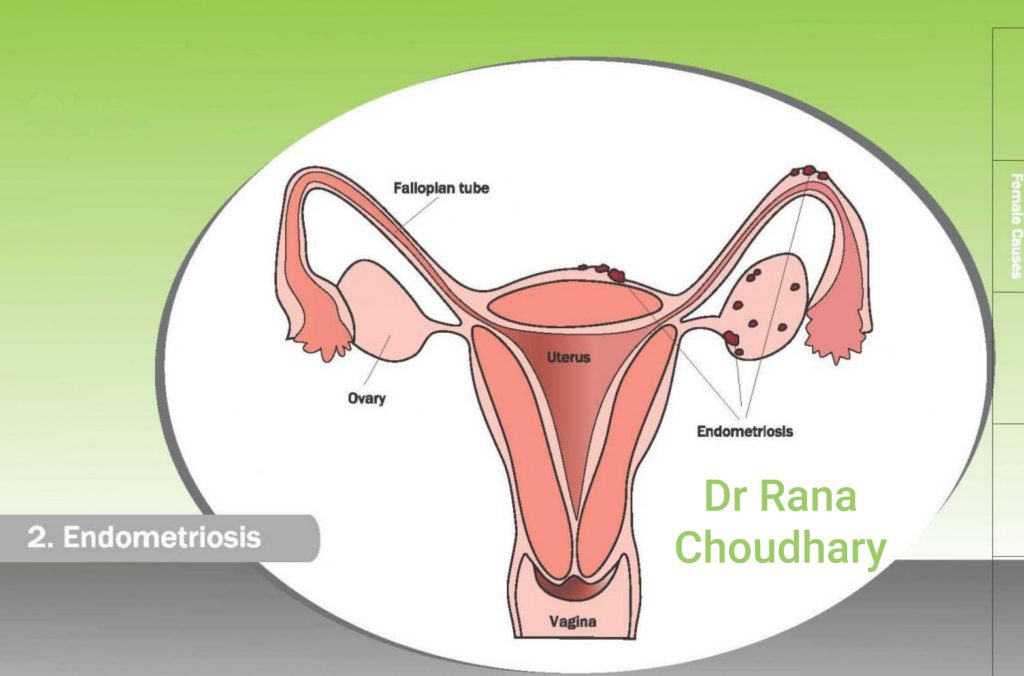
ENDOMETRIOSIS
What is Endometriosis?
- Endometriosis is a common condition that affects women during the reproductive years. Endometriosis is a condition where tissue, similar to the one that normally grows inside the uterus (lining of uterus), also grows outside of the uterus. The tissue inside the uterus is called “endometrium” and the tissue outside of the uterus is called “endometriosis”. The most common places where endometriosis occurs are the ovaries, the fallopian tubes, the bowel, and the areas in front, in back, and to the sides of the uterus.
- If you have severe pain during menses and also having some trouble in conceiving then you may be having endometriosis. While some women with endometriosis have severe symptoms some may have few or no symptoms.
- There is no cure for endometriosis, but there are several treatment options. The best treatment depends on your individual situation which can be judged by your infertility specialist.
- The treatment is custom made for each individual depending upon the symptoms and severity of the condition. Such individualization gives the best results to our patients.
What are the causes of endometriosis?
- The cause of endometriosis is not known.
- A common theory is that some menstrual blood and endometrial flows backwards through the fallopian tubes and into the pelvis during a menstrual period. Normally these tissues are taken care by our immune system and hence most of the women don’t develop endometriosis; unfortunately some women have failure of these immune system and the endometrial tissues persist in the pelvic organ. This later on gets blood supply from the surrounding organs and stars growing in each cycle under the influence of the hormones and starts producing symptoms . This tissue then grows where ever it lands in the pelvis. This is called the retrograde menstruation theory. It explains external endometriosis. As the bleeding occurs from the endometriotic tissue and is on the surface of the organs, hence leads to adherence of the organs leading to alteration in the relationship between the fallopian tubes and ovaries, and thereby difficulty in conception.
- In some cases internal endometriosis is seen. The Germ line theory explains it. In these cases the endometrium grows internally due to the germ cells that grow in this abnormal location causing endometriosis. In these women, the bleeding occurs within the ovarian tissue, hence mostly these women do not have any symptoms of the disease. It remains silent for a long time till the internal damage due to cyclic bleeding and ovarian blood filled cyst ( chocolate cyst ) formation takes places. This can then be diagnosed on ultrasonography (USG). However by this time due to damage to the ovarian tissue the ovarian reserve gets diminished, which can be seen by the low AMH (Anti Mullerian Hormone) levels in these women. If it is not treated timely, then it will further decrease the ovarian reserve and hence hamper the chances of conception.
- There are several other theories. However it is best to focus on treatment rather than cause in cases of endometriosis.
How does endometriosis cause infertility?
There are many ways in which endometriosis affects fertility.
- Anatomical distortion – Moderate to severe endometriosis causes damage to the ovaries or fallopian tubes which leads to fibrosis and scarring. This may lead to anatomical distortion of the fallopian tubes leading to blockage of the fallopian tubes or any obstruction between the fallopian tube and ovaries.
- Immunological aspects – It has been seen that even in mild cases of endometriosis the women produce antibodies against the sperm or even the egg and embryo in the fluid around the uterus leading to infertility. Further, there is imbalance between the TH1 and TH2 cells which hampers implantation and may lead to abortions.
- Quality of egg / oocyte – some cases of mild degree and sever degree of endometriosis the quality of female egg is also compromised leading to compromised oocyte ,embryos and abnormal implantation leading to infertility or even abortions.
- Interlukin (IL) induced damage of gametes – Endometriosis causes release of toxic Interlukins(ILs) and Cytokines(CKs) in the woman. These adversely affect both the sperm as well as the egg or ova leading to their damage and hence difficulty in conception.
What are the symptoms associated with endometriosis?
- 1. Pain during menses (Dysmenorrhoea) —
- Pelvic pain caused by endometriosis can occur:
- Just before or during the menstrual period. In some women, painful periods get worse over time (Dysmenorrhoea)
- Between menstrual periods, with worsened pain during the period
- With bowel movements or while urinating, especially during the period
Pelvic pain can also be caused by many other conditions, such as pelvic infections and irritable bowel syndrome. A gynaecologist can help to figure out if endometriosis may be the cause of your pain.
Some women experience severe pain during or just after intercourse/ sex due to endometriosis induced adhesions and scarring between the pelvic structures.
Endometriosis can make it more difficult to become pregnant. This might occur because endometriosis causes scar tissue to develop, which can damage the ovaries or fallopian tubes. Even women with endometriosis who do not have scar tissue can have difficulty becoming pregnant due to reasons explained above. However, in women who become pregnant, endometriosis does not harm the pregnancy. Symptoms of endometriosis often improve after pregnancy.
Some women do not have any major symptoms or complaints other than just a few days of premenstrual spotting.
Some women do not have any symptom of endometriosis and are diagnosed to have a blood filled cyst incidentally on USG. This cyst is called as an endometrioma. Endometriomas are usually filled with old blood that resembles chocolate syrup; thus, they are sometimes called chocolate cysts. Endometriomas are sometimes seen during a pelvic ultrasound or felt during a pelvic exam.
Sometimes if there are endometriotic deposits in the bladder or bowel region then the women may have bleeding while passing urine or even blood in stools.
How is endometriosis diagnosed?
- Endometriosis may be suspected if the woman has any of the above symptoms.
- Clinical examination by your infertility specialist can help further confirm endometriosis.
- On clinical examination during per vaginal (PV) examination, uterus may be fixed due to scarring of endometriotic tissue and adhesions between the surrounding structures. There may be nodularity or scarring felt in the pouch of doughlas. Sometimes the enlarged chocolate cyst can also be felt on PV examination.
- In other cases a pelvic ultrasound may reveal endometriosis in the form of persistent fluid collection in the pouch of douglas (suggestive of endometriosis), endometrioma which are type of ovarian cyst or rarely if there are dense adhesions. These have a homogenous appearance and hence can be easily distinguished from other ovarian cysts.
- For example:
- A simple ovarian cyst will appear as completely dark structure.
- A corpus luteal hematoma will have a classical honey comb appearance.
- And a solid tumor will appear more white on USG.
- In some cases for differentiation a CTscan or MRI may be required.
- However, the only way to know for sure if you have endometriosis is to have surgery. Symptoms of the patient do not routinely point towards the severity of the disease as women with mild disease can have severe symptoms, and women with severe disease can have mild symptoms. Endometriosis is considered mild, moderate, or severe depending on what is found during surgery.
- During surgery the endometriosis can be divided into 4 stages depending upon the severity, with stage 1 being the mildest form of endometriosis and stage 4 the severest form. Treatment is based on the staging of endometriosis.
What are the different stages of endometriosis?
- The American Society for Reproductive Medicine (ASRM) classification system for endometriosis is the most accepted.
- Endometriosis is classified into one of four stages: I-minimal, II-mild, III-moderate, and IV-severe.
- This classification depends on location, extent, and depth of endometriosis implants; presence and severity of adhesions; and presence and size of ovarian endometrioma.
- A majority of women have minimal or mild endometriosis, which is characterized by mild adhesions and superficial implants.
- Moderate and severe endometriosis is characterized by chocolate cysts and more severe adhesions.
- The stage of endometriosis does not correlate with the presence of or severity of symptoms; with stage IV endometriosis, infertility is very likely.
- However, unfortunately no staging system correlates well with the chance of conception following therapy. This poor predictive ability is related to the arbitrary assignment of point scores for pathology and arbitrary cut off.
What are the treatment options available?
- There are many treatment options for endometriosis. But the treatment depends on many factors such as age of the women, desire for fertility, need of contraception, severity of symptoms, extent of endometriosis (excessive involvement of bowel or bladder) and last of all patient’s desirability. So the treatment has to be tailor made for a particular woman.
- However here we will be discussing management of endometriosis related to fertility. Medical management with pain killers or oral contraceptive pills is not suitable for these patients. In some cases GnRh injections are given to relieve from symptoms but again these are not advisable in women who desire fertility.
- Pain killers just give temporary relief and do not treat endometriosis.
- Oral contraceptives help by preventing menses and hence bleeding within the pelvis. Hence the endometriotic patches do not bleed and then die out provided the pills are taken continuously for months together. However in such case, the pregnancy is then further postponed as there is no ovulation and endometrial development. Therefore these treatment options are not useful and desired by the patients who are anxious to conceive.
- Gn Rh injections also have a similar mechanism of action and are detrimental to the endometrium. Hence cannot be used in infertility patients.
- The best protocol of management in infertile patient is usually surgical clearance followed by ovulation induction and IUI or IVF-ICSI in very severe disease. Many a time surgical clearance is followed by spontaneous pregnancies also. However sometimes ovulation induction with planned relations or IUI can precede surgical intervention with good pregnancy rates. In some cases of severe disease wherein there is spread to bladder or rectum an IVF cycle may be planned without clearing the disease completely. The decision of treatment has to be taken by the doctor and couple after understanding the pros and cons.
- Research has not firmly proved that removing mild endometriosis improves fertility. For moderate to severe endometriosis, surgery will improve your chances of pregnancy. In some severe cases, a fertility specialist will recommend skipping surgical removal and using IVF.
- Generally in Stage 1 and 2 of endometriosis management includes gonadotrophin stimulated 3 to 6 cycles of intra uterine insemination (IUI) depending upon the age of the woman and her AMH levels. In severe cases of endometriosis like Stage 3 and 4, surgery is followed by gonadotrophins. In these cases the success rate in terms of pregnancy following an IUI is generally poor around 5%. Hence, in such women better results are achieved by using prev IVF GnRh therapy for 4-6 months followed by IVF or ICSI.
Stage 1 | 3 to 6 cycles of Gonadotrophin stimulated intra uterine insemination (IUI) |
|---|---|
Stage 2 | 3 to 6 cycles of Gonadotrophin stimulated intra uterine insemination (IUI) |
Stage 3 | Surgery is followed by Pre IVF gonadotrophins may be tried. This will be followed by ovulation induction and IVF-ICSI |
Stage 4 | Surgery is followed by Pre IVF gonadotrophins may be tried. This will be followed by ovulation induction and IVF-ICSI |
How is endometriosis managed laparoscopically?
- Laparoscopy is the most common procedure used to diagnose and remove mild to moderate endometriosis. Instead of using a large abdominal incision, the surgeon inserts a lighted viewing instrument called a laparoscope through a small incision. If the surgeon needs better access, he or she makes one or two more small incisions for inserting other surgical instruments.
- The internal organs are examined to look for signs of endometriosis (dark blackish or brownish powdery spots, also called as gun powder appearance) and other possible problems like adhesions or blood filled cysts. Any visible endometriosis implants and scar tissue that may be causing pain or infertility are removed. Removal of endometriosis or scar tissue involves using one of the various techniques, including cutting and removing tissue (excision) or destroying it with a laser beam or electric current (electrocautery).
- If an endometriosis cyst is found growing on an ovary (endometrioma), it is likely to be removed. There are various ways of surgically treating an endometrioma, including draining it, cutting out part of it, or removing it completely (cystectomy). Any of these treatments brings pain relief for most women but not all. Cystectomy is most likely to relieve pain for a longer time, prevent an endometrioma from growing back, and prevent the need for another surgery.
- During surgery there is bleeding from the endometriotic patches/ spots. Traditionally cauterisation of these spots have been done. But these lead to increase in post op adhesions and scarring of the pelvic organs. Some surgeon use suturing of the ovarian cyst base to minimise this adhesion, however the bleeding may still continue. Recently many surgeons are using hemostatic agents like interseed etc over the base of the ovary giving variable results. This helps in controlling the oozing over the raw surface and also prevents future adhesion formation.
What are the risks and complications involved?
- The complications are more or less similar to any laparoscopic surgery. However in case of extensive endometriosis there is a slightly more chance of organ injury.
- In some instances minimal to mild endometriosis spots may not be seen during a laparoscopy surgery and these may flare up later during treatment and may need additional surgery.
Why and How to prevent recurrence of endometriosis ?
- Management of infertility along with endometriosis can be long and tiring for some patients. It is seen that some women do not continue the treatment of endometriosis, but this has severe repercussions and can lead to extensive endometriosis and scarring. Few women after undergoing the surgery and 3 to 4 few IUI cycles, if they do not conceive then become frustrated and stop the treatment . This leads to recurrence of endometriotic lesions and further damage to the tubes and ovaries.
- If the couple/ woman is exhausted physically or mentally and wants to a break then it is a good idea to take some simple medications like hormonal pills eg.
- Oral contraceptive pills continuously for months together so that she does not get her menses and future endometriosis can be avoided.
- Progesterone supplementation can also be used for shorter duration of period in woman planning for conception as this will prevent further endometriosis and if in case the women becomes pregnant it will benefit the pregnancy too.
- However, waiting for too long is not advisable in cases of endometriosis as it further lowers the chances of getting pregnant.
- Another important aspect is that women with endometriosis have shown to have an adverse pregnancy outcome as compared to women who do not have endometriosis. Hence vigilant monitoring and care during pregnancy is also very important.
I am 21 years and have been diagnosed with endometriosis. Will it affect my chances of getting pregnant in future? How long can I postpone my pregnancy?
- Yes, endometriosis affects the changes of getting pregnant adversely. Studies have shown that the endometriotic lesions and cysts go on increasing in size if not treated and will damage the normal architecture and functioning of the reproductive organs.
- Endometriotic/ chocolate cysts damage the normal ovarian tissue and hence reduce the ovarian reserve. Studies have shown that in untreated cases , over a period of time the AMH (Anti mullerian hormone ) values go on decreasing. (AMH is a marker of ovarian reserve).
- However, if the women still wants to postpone or take a break then oral progesterone like Dydrogesterone can be used. This is a new and unique molecule which will prevent bleeding by preventing endometrial shedding. However it does not interfere with the endometrial development and is not toxic to the embryo. It infact supports pregnancy, in case the women gets naturally / spontaneously pregnant during this waiting period.
- To summarise , waiting for too long is not advisable in cases of endometriosis as it further diminishes the chances of pregnancy due to ovarian damage and tubal adhesions formation.
I am 28 years old, married and have undergone surgical excision of chocolate cyst 2 months back. I am tired of the prolonged treatment for infertility and endometriosis. What should I do?
- If the couple/ woman is exhausted physically or mentally and wants to a break then it is a good idea to take some simple medications like hormonal pills eg.
- Oral contraceptive pills continuosly for months together so that she does not get her menses and future endometriosis can be avoided.
- Progesterone supplementation can also be used for shorter duration of period in woman planning for conception as this will prevent further endometriosis and if in case the women becomes pregnant it will benefit the pregnancy too.
- However , waiting for too long is not advisable in cases of endometriosis as it further diminishes the chances of pregnancy due to ovarian damage and tubal adhesions formation.
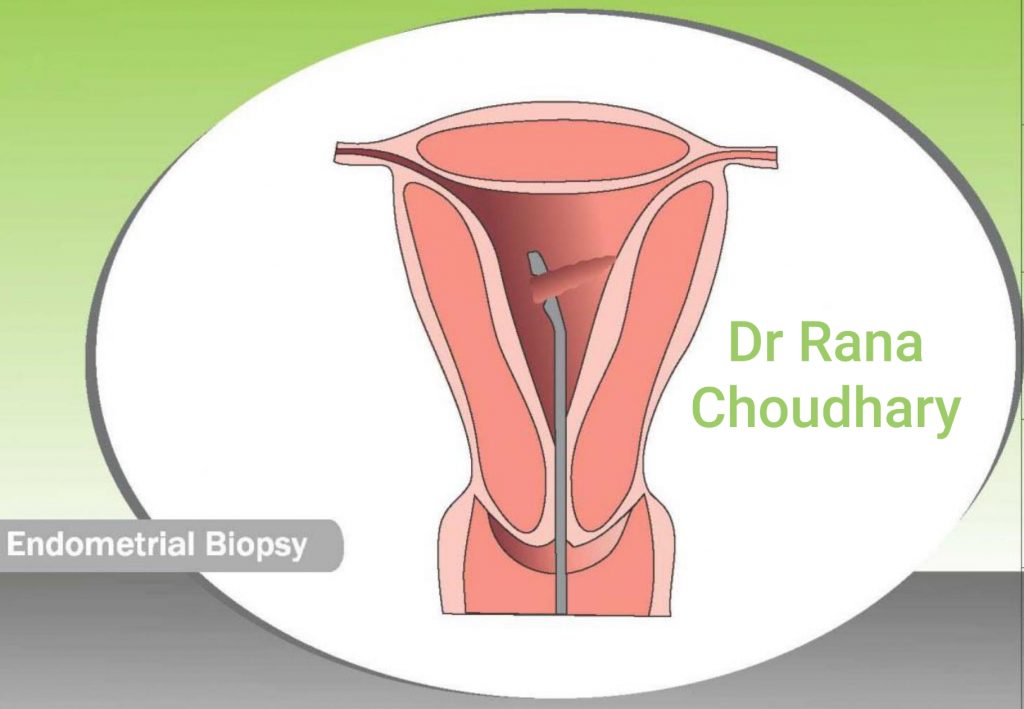
Endometrial polyps or endometrial hyperplasia
These may cause heavy bleeding during menses and can be easily treated using endometrial biopsy or endometrial curettage also known as D & C. This is a day care procedure and patient can go home the same day. The endometrial biopsy sample can be sent for histopathological examination for knowing the exact causes of heavy menstruation / bleeding.